Custom Scleral Lenses:
When corneal irregularity is extreme, scleral lenses are preferred over other lens designs. These lenses vault over the cornea, aligning with the sclera and overlying conjunctiva (white of the eye). Scleral lenses can overcome nearly any corneal irregularity and should be considered as an option prior to referral for corneal transplantation. Individuals who have keratoconus and who otherwise would have undergone corneal transplantation secondary to contact lens failure can achieve success with these lenses. These lenses are can be designed with an abundance of unique modifications. Advanced fitting techniques can include impression based and scan based design. These lenses are lathe-cut and can be produced in an extensive range of shapes, diameters, materials, and nearly endless refractive powers. In addition, highly customizable optics such as wavefront guided, higher order aberration correcting optics can be added in some lenses.
Custom Scleral Lenses & Prosthetic Scleral Devices

Scleral lenses and scleral devices are specially designed to rest on the conjunctiva and underlying sclera, the “white” of the eye, and vault over the entire corneal surface.
The cornea focuses light and when diseases, such as keratoconus, trauma or surgery distorts its shape it also distorts vision. The cornea is also one of the most sensitive tissues in the body and the one most damaged by dry eye and ocular surface disease. By vaulting over the cornea, the lens masks the irregular shape. The space created between the cornea and the back surface of the device is space is filled with fluid. In ocular surface disease and this fluid reservoir acts as a “tear bandage” which bathes the corneal surface to provide comfort, protection, and healing for people with diseases that affect the ocular surface. This therapeutic use can rehabilitate the cornea and prevent further damage caused by various diseases.
Scleral lenses can be a great option for those with irregular corneas and ocular surface disease. Many times these lenses are the only option for patients with severe disease and often times can delay or prevent the need for surgical intervention. Occasionally standard scleral lenses will be unsuccessful due to the complex shape of the eye. In those cases custom scleral lenses and prosthetic scleral devices become the best option.
Dr. John D. Gelles works extensively with these devices and has helped suffering patients from all over the world. He has been instrumental in developing advanced technology, fitting techniques and lens designs. Custom made scleral lenses, whether derived from diagonic fitting, software driven, scan based or impression based data, all can lead to a successful result. As an expert in these techniques, Dr. Gelles determine which approach will be best so he can create a custom scleral lens or device to meet your individual needs.
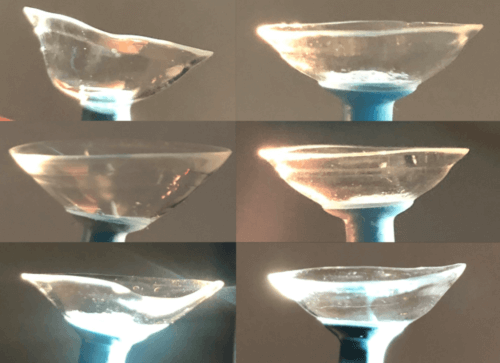
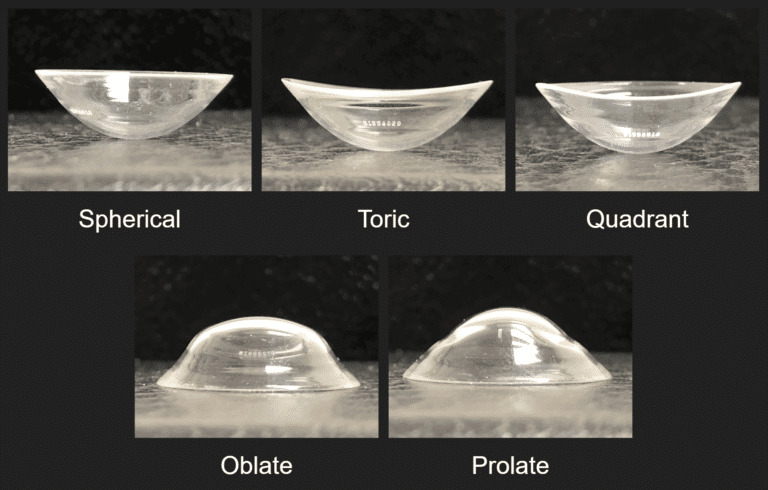
A variety of custom made scleral lenses, each is made to mimic the ocular shape of the patient’s eye. Note no 2 lenses are the same just as no 2 eyes are the same. Image by John D. Gelles, O.D. Copyright © 2020 by the Cornea and Laser Eye Institute. All Rights Reserved.

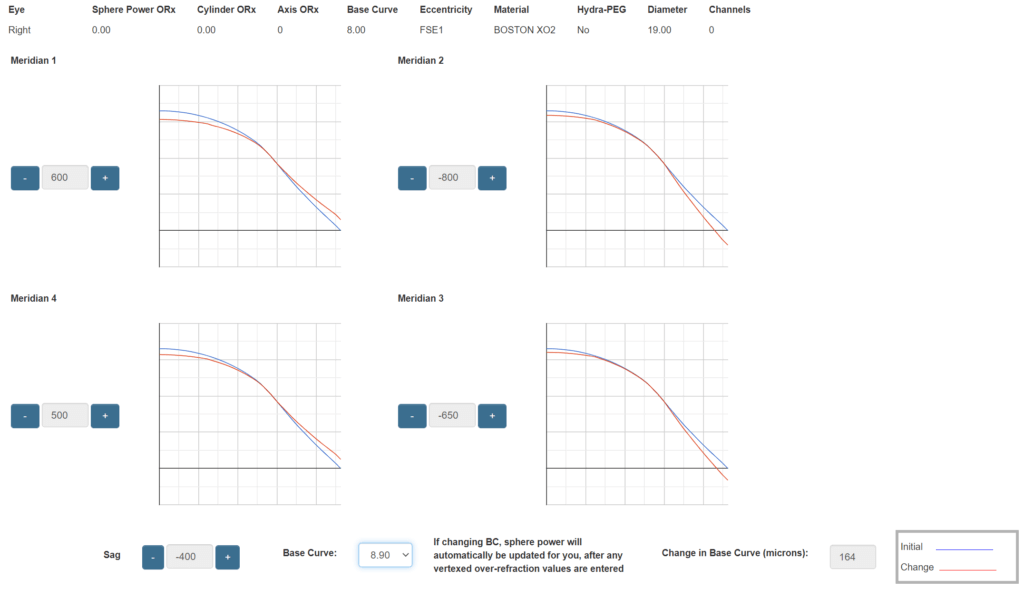
Software Driven Scleral Lenses
The classic way to fit and design scleral lenses is by use of a diagnostic contact lens set. A series of lenses with varying curvatures are placed on the eye. The alignment of the lens is evaluated and during the design process modification to the lenses are made based on the observations and on eye performance. The majority of diagnostic designs have simplified parameter options, which can limit the design process. Scleral lens design software can remove these restrictions, allowing for more customized lenses to be made. Several custom scleral lenses or scleral devices, such as a PROSE device, use these powerful software programs allowing Dr. Gelles to create more customized of lenses.
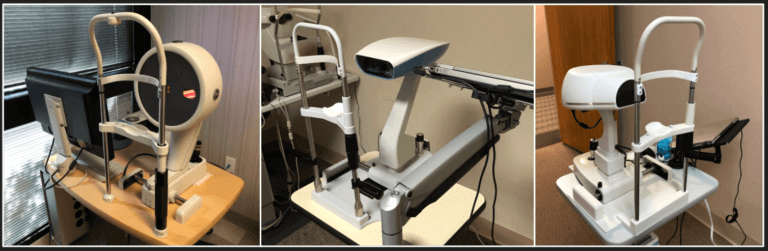
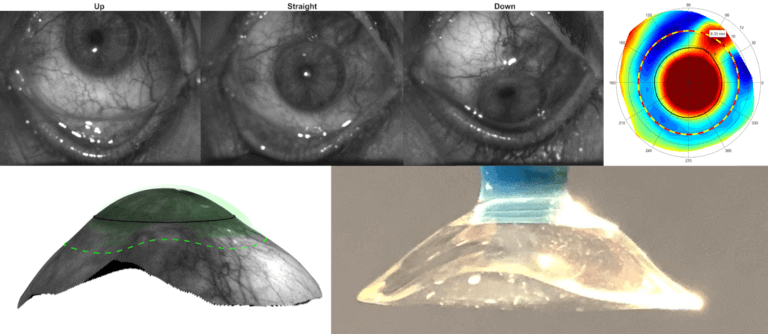
Scan Based Scleral Lenses
Another design approach uses highly specialized devices to scan the ocular shape. This shape data is used to create a 3 dimensional digital model of the eye. Once this model is created Dr. Gelles will use a specialized computer aided design software to create a lens unique to the contour of the eye.
Wavefront Guided Scleral Lenses
In many cases vision with scleral lenses, though improved, may still have some residual aberrations. These residual aberrations are called an higher order aberration. They are responsible for doubled, overlapped, ghosted vision with glare, flare, starburst and halos. In these cases, the addition of highly customized wavefront guided higher order aberration correcting scleral lenses can further improve your vision.
Vision Simulations of Traditional Scleral Lenses & Wavefront Guided Scleral Lenses
These optics are considered High Definition optics as the clarity is improved over traditional optics. These optics have been studied in university based laboratory settings over the past 10 years and only recent have made it to practice. At the Cornea and Laser Eye Institute, Dr. Gelles as found these lenses provide an average 50% percent reduction in aberrations and 1 or more lines of visual acuity improvement. Dr. Gelles is currently running a clinical trial to evaluate vision improvements with this technology.
Indications for Custom Scleral Lenses & Prosthetic Scleral Devices
Irregular Corneal Conditions:
Corneal Ectasia: These are diseases characterized by weak and thin corneal tissue resulting in an irregular cornea shape. Examples include conditions such as keratoconus, keratoglobus, pellucid marginal degeneration, and corneal ectasia after surgery.
Post-Keratoplasty: A keratoplasty is also known as a corneal transplant. These surgeries are used when the cornea is severely scarred or have extremely advanced disease. They can involve the replacement of all or select layers and areas of the cornea. After transplantation the cornea is smoother and clearer but irregularities still exist. Examples include penetrating keratoplasty (PK), deep anterior lamellar keratoplasty (DALK), corneal tectonic grafts (patch grafts), and epikeratophakia.
Post-Corneal Surgery: In very rare cases, after a corneal procedure to reshape the cornea, the corneal surface may become irregular in shape. Examples include after laser assisted in situ keratomileusis (LASIK), photorefractive keratectomy (PRK), radial keratotomy (RK), or intracorneal ring segment (Intacs, Keraring, MyoRing, Ferrara Ring).
Corneal Opacity: A corneal opacity is a scar in the cornea. Scars may result in an irregular corneal surface and can occur after trauma, infection, or advanced ectasia.
Corneal Dystrophies: These are genetic, often progressive, conditions where abnormal tissue often accumulates in the cornea. Anterior and stromal dystrophies such as lattice, granular, Meesmann, Cogan, and Reis-Bucklers dystrophies may result in an irregular corneal shape.
Corneal Degenerations: These conditions cause deterioration and sometimes impair function of the peripheral cornea tissue. Examples include Salzmann’s nodular degeneration and Terrien’s marginal degeneration
Ocular Surface Diseases:
Ocular Surface Disease: These diseases are generally caused by problems with inflammation on the eye surface. This can result from ocular chronic graft versus host disease (GVHD), after radiation therapy, Sjogren’s syndrome, rheumatoid arthritis, or dry eye induced by autoimmune or other diseases which attack the lubrication secreting glands of the eye.
Limbal Stem Cell Deficiency: Generally caused by intense immune system reactions or burns, these conditions may result in severe scarring to ocular membranes and damage cells responsible for corneal healing. Scarring of eye tissues result in mechanical or friction damage. Conditions such as Stevens–Johnson syndrome (SJS), ocular cicatricial pemphigoid, mucous membrane pemphigoid, chemical or thermal burn injuries are the cause.
Neurotrophic Keratitis: Reduced corneal nerve function resulting in a lack of corneal sensation. This can lead to corneal damage and poor healing. This can happen with or after conditions such as herpes zoster (shingles), herpes simplex (ocular herpes), familial dysautonomia, trigeminal nerve dysfunction which may lead to persistent epithelial defects (PED) or corneal wounds that don’t heal.
Exposure Keratitis: This type of ocular surface disease is caused when an eye can not completely close. This exposure causes severe localized dryness which leads to the breakdown of the cornea and ocular surface tissue. This can happen after surgery (after blepharoplasty or lid repair), lagophthalmos, anatomic lid malposition, paralytic exposure (after stroke or intracranial surgery), or acoustic neuroma.



