Understanding Keratoconus and the Need for Surgical Intervention
Keratoconus is a progressive eye condition where the cornea, the clear front part of the eye, thins and bulges into a cone-like shape. This irregular shape can cause significant vision problems, including blurred and distorted vision, sensitivity to light and glare, and difficulty driving at night. While mild cases of keratoconus can often be managed with corrective lenses or corneal crosslinking, more advanced cases may require surgical intervention to restore vision and prevent further deterioration.
Traditionally, keratoplasty, or corneal transplant surgery, has been the go-to treatment for advanced keratoconus. However, in recent years, a new and innovative approach known as corneal tissue addition keratoplasty (CTAK) has emerged as a promising alternative. In this article, we’ll explore the differences between traditional keratoplasty and CTAK, as well as the role of femtosecond laser technology in these corneal surgeries.
Traditional Keratoplasty: An Overview of Penetrating Keratoplasty
Penetrating keratoplasty (PK) is the most common type of traditional keratoplasty procedure for treating keratoconus. During a PK surgery, the surgeon removes the central portion of the patient’s cornea and replaces it with a donor cornea. This procedure is typically performed under local or general anesthesia and can take several hours to complete.
The recovery process for PK can be lengthy, with patients often experiencing blurred vision, sensitivity to light, and the need for sutures that remain in place for at least 6 months to one year. Additionally, there is a risk of rejection, where the patient’s immune system attacks the donor cornea, which can lead to the need for additional surgeries or even vision loss.
Corneal Tissue Addition Keratoplasty (CTAK): A Revolutionary Approach to Treating Keratoconus
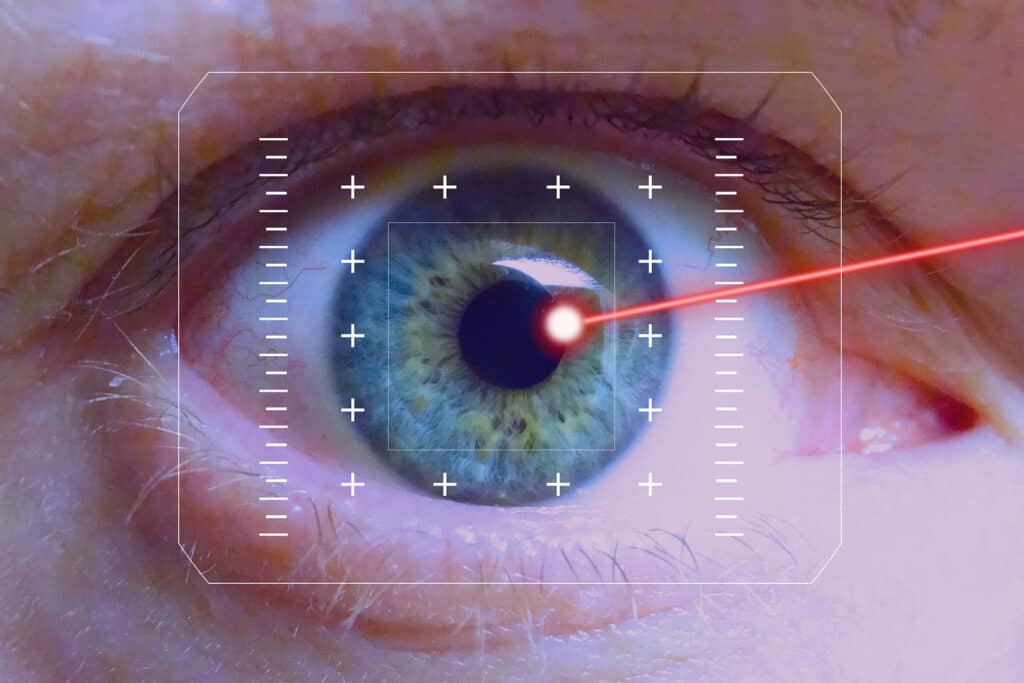
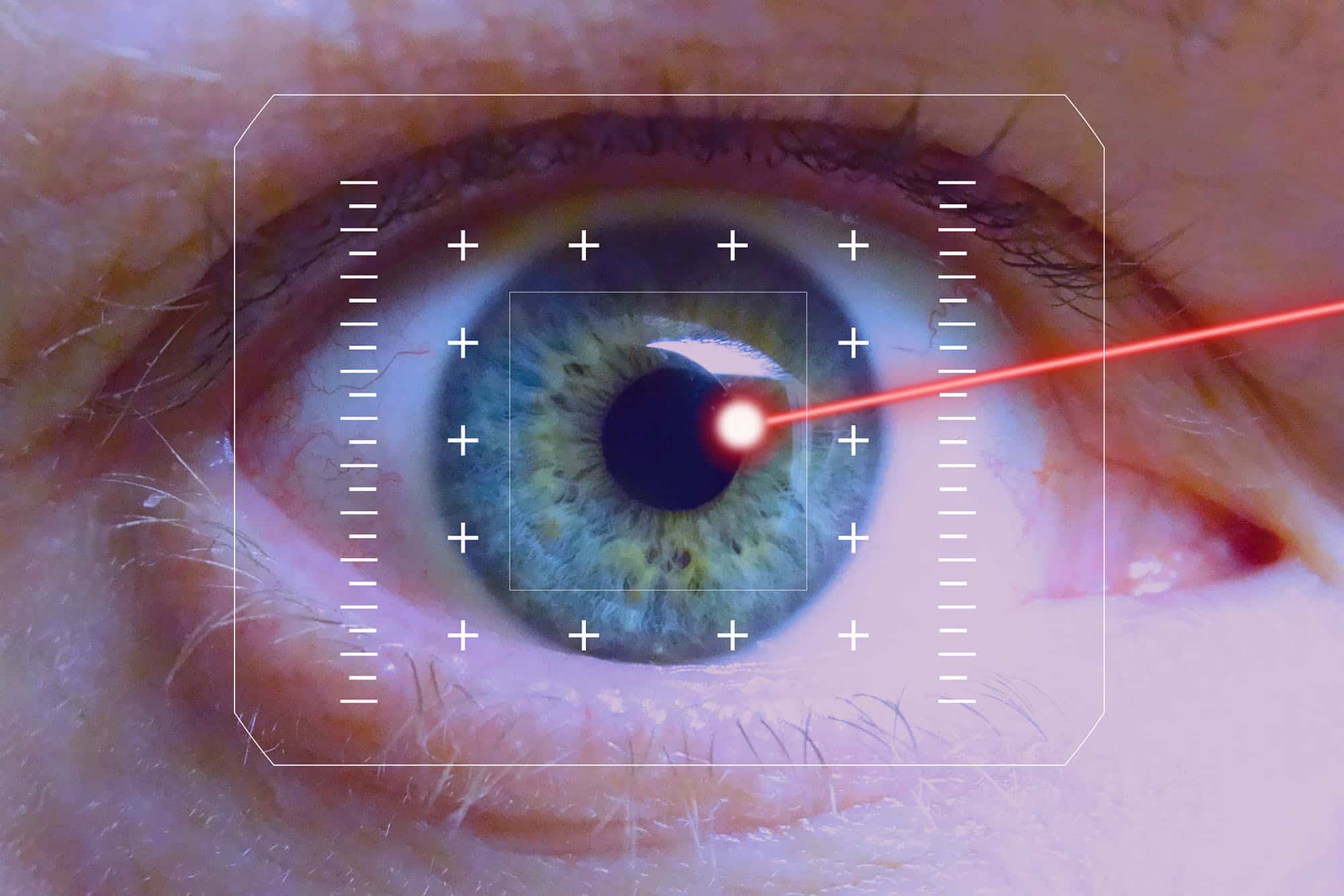
In contrast to traditional keratoplasty, corneal tissue addition keratoplasty (CTAK) is a relatively new and innovative procedure, developed at the Cornea and Laser Eye Institute, that aims to address keratoconus without the need for a full corneal transplant. During a CTAK procedure, the surgeon uses a femtosecond laser to create a small, precise channel within the cornea and then inserts a custom shaped sterilized corneal tissue inlay in the channel to reshape the cornea.
The key advantages of CTAK include:
- Preserving the Patient’s Natural Cornea: CTAK allows the surgeon to maintain the patient’s natural corneal tissue, which can lead to a faster recovery and a lower risk of rejection compared to traditional keratoplasty.
- Improved Visual Outcomes: The customized corneal tissue inlay used in CTAK can help correct the irregular shape of the cornea, resulting in improved visual acuity and reduced distortion.
- Less Invasive Surgery: CTAK is generally a shorter and less invasive procedure than traditional keratoplasty. It can be performed in the office rather than in a surgery center or hospital, with a quicker recovery time for the patient.
- Potential for Reversibility: In some cases, the corneal tissue inlay used in CTAK can be removed or replaced if needed, offering more flexibility than a traditional corneal transplant.
Comparative Analysis: CTAK vs. Traditional Keratoplasty
When comparing CTAK and traditional keratoplasty, there are several key factors to consider:
- Surgical Approach
- CTAK: Less invasive procedure that preserves the majority of the patient’s natural cornea.
- Traditional Keratoplasty: Involves the removal and replacement of the central portion of the cornea with a donor cornea.
- Visual Outcomes
- CTAK: Potential for improved visual acuity and reduced distortion due to the customized corneal tissue inlay.
- Traditional Keratoplasty: Potential for improved visual acuity and reduced distortion, with generally more variability in the visual outcomes, with some patients experiencing improved vision and others still struggling with visual distortions.
- Recovery Time
- CTAK: Generally a shorter recovery time compared to traditional keratoplasty, with less disruption to the patient’s daily life. There are usually no sutures used for the CTAK procedure.
- Traditional Keratoplasty: Longer recovery time, with the need for sutures that remain in place for several months.
- Rejection Risk
- CTAK: Lower risk of rejection compared to traditional keratoplasty, as the patient’s natural corneal tissue is largely preserved and the inlay is cut from a sterilized corneal tissue.
- Traditional Keratoplasty: Higher risk of rejection or failure over time, as the patient’s immune system may attack the donor cornea.
- Reversibility
- CTAK: In some cases, the corneal tissue inlay used in CTAK can be removed or replaced if needed, offering more flexibility.
- Traditional Keratoplasty: Once the corneal transplant is performed, it is a permanent procedure, with limited options for reversal or modification.
Managing Keratoconus: Treatment Options Beyond Surgery
While surgical interventions like CTAK and traditional keratoplasty are often necessary for advanced cases of keratoconus, there are other treatment options that can be effective in managing the condition. In fact, a comprehensive keratoconus treatment plan will likely include more than one method to improve visual acuity and stabilize the cornea. These may include:
- Corrective Lenses: Glasses or contact lenses can be used to correct the refractive errors caused by the irregular corneal shape.
- Corneal Crosslinking: This procedure uses UV light and a photosensitizing agent to strengthen the corneal structure and slow the progression of keratoconus.
- Topography Guided PRK: This procedure uses the excimer laser and the individual map of each patient’s cornea, to create a more regular corneal shape..
- Intrastromal Corneal Ring Segments: Intacs are small, curved implants that can be inserted into the cornea to help reshape and flatten the corneal surface.
Conclusion
When it comes to treating keratoconus, there is no one-size-fits-all solution. The choice between traditional keratoplasty and the newer CTAK procedure will depend on a variety of factors, including the severity of the patient’s condition, their overall eye health, and their personal preferences and lifestyle.
If you or a loved one is struggling with the effects of keratoconus, we encourage you to schedule a consultation at the CLEI Center for Keratoconus to discuss your treatment options with one of our experienced ophthalmologists. By understanding the pros and cons of each approach, you can make an informed decision that aligns with your unique needs and goals for enhanced vision and quality of life.