Keratoconus, a progressive eye condition characterized by the thinning and bulging of the cornea, presents a significant challenge in the field of ophthalmology. For individuals afflicted with this disorder, the distorted shape of the cornea can lead to visual impairment and a diminished quality of life. While traditional treatments such as glasses, specialty contact lenses, and in severe cases, corneal transplants, have provided relief for many patients, there remains a need for innovative approaches that offer improved outcomes and reduced risks.
In 2016, clinical trials began on a promising procedure: corneal tissue addition keratoplasty (CTAK). This groundbreaking technique, which was developed and pioneered right here at CLEI, involves augmenting the corneal structure with additional tissue to reinforce its integrity and restore vision. Unlike treatments that focus solely on correcting refractive errors, corneal tissue addition addresses the underlying structural irregularity associated with keratoconus.
In this article, we delve into what’s involved in a comprehensive keratoconus treatment plan, the mechanisms behind corneal tissue addition therapy, and how it compares to other corneal reshaping procedures. By taking a closer look at CTAK, we aim to shed light on the transformative potential of this innovative approach in the management of keratoconus.
Comprehensive Keratoconus Treatment: What’s Involved?
To improve the quality of life for our keratoconus patients, we take a comprehensive, three-step approach to treating this progressive disease. Each of the three steps is important for a patient who wants to stop the progression of the disease and see as clearly as possible. A brief overview of these three steps will help you to understand where corneal tissue addition keratoplasty fits into a keratoconus treatment plan.
Step 1: Halt the Progression of Keratoconus
In 2008, we began treating patients with corneal crosslinking (CXL) as part of the initial clinical studies that took place in the US. Crosslinking quickly became one of the most important advancements in keratoconus treatment. This procedure involves administering riboflavin (Vitamin B2) in conjunction with ultraviolet A light (UVA-365nm). The interaction of riboflavin and the UV light causes the cornea to stiffen, making it more resistant to disease progression over time, which in turn helps preserve a patient’s vision. At CLEI, we offer standard and specialty crosslinking treatments.
Step 2: Improve the Cornea’s Shape
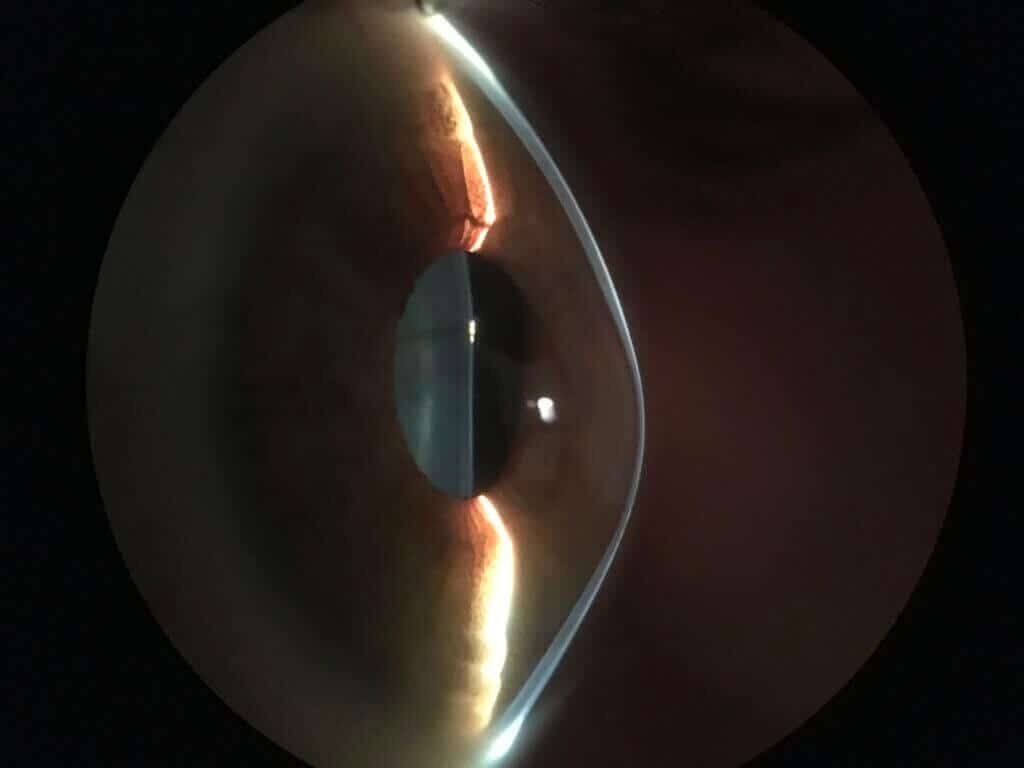
Keratoconus causes a corneal shape deformation. Instead of presenting a normal symmetrical dome shape, the eye begins to bulge at the area where the cornea is thinnest, creating an asymmetrical cone-like shape. This can cause a multitude of refractive errors. Keratoconus patients often report visual distortions including glare and halos, flares, smears, overlapping images, multiple images, ghosting, streaking, and starbursts. To address these issues, patients can undergo procedures designed to improve corneal shape. Not every keratoconus patient needs a reshaping procedure, however, many patients can benefit from one of the following procedures:
- Corneal Tissue Addition Keratoplasty (CTAK): During this procedure, we use a custom-shaped inlay of gamma-irradiated corneal tissue, placed in a channel created by the femtosecond laser to reshape the cornea and improve vision.
- Topography-Guided PRK (TG-PRK): In select patients with keratoconus, topography-guided PRK may be a good option. For this procedure, an excimer laser is used to reshape the cornea and reduce corneal irregularity, for improved quality of vision in glasses and potentially soft contact lenses.
- Intracorneal Rings (Intacs): FDA-approved in 1998 for nearsightedness and later under a human device exemption for keratoconus treatment, Intacs are implantable intracorneal ring segments (ICRS) made of polymethylmethacrylate (PMMA), an inert polymer used in eye surgery for many years. With keratoconus patients, Intacs are used to reshape the cornea. The thickness and position of the Intacs segments are chosen based on individual corneal shape. One or two segments may be placed in the cornea, depending on the patient’s unique measurements.
- Corneal Transplant: In advanced cases of keratoconus, corneal transplantation may be necessary, especially when dense scarring is present. During a corneal transplant, diseased corneal tissue is removed from the patient’s eye and replaced with donated corneal tissue. At CLEI, we perform both full-thickness transplants called a penetrating keratoplasty (PK), and partial-thickness transplants, called deep anterior lamellar keratoplasty (DALK). We specialize in using the femtosecond laser to create additional precision for a corneal transplant procedure.
To learn whether you could benefit from one of these procedures, a thorough evaluation with one of our CLEI doctors is key. At CLEI, our doctors are experts and innovators who perform all of these procedures. They can select the correct corneal reshaping treatment to optimize your cornea and vision. Feel free to request an appointment with us for a personal evaluation.
Step 3: Improve Keratoconus Vision
The third and final step in keratoconus management is to improve vision. This can be done both surgically and non-surgically. Potential treatment options include PRK, implantable collamer lenses (EVO ICL), or specialty contact lenses. Our CLEI doctors can create a customized treatment plan to help you achieve the best possible vision that includes one of these options.
How CTAK Compares to Other Corneal Reshaping Procedures
CTAK is a valuable tool for reshaping an irregularly shaped cornea. While not every patient will be a candidate for CTAK, this procedure does offer several benefits for those who do qualify.
CTAK Vs. Topography-Guided PRK
CTAK and topography-guided PRK are two very different procedures, but both have the goal of reshaping the cornea to reduce refractive errors. One big difference between the two is that CTAK is fully reversible, whereas topography-guided PRK is a permanent procedure. If CTAK proves unsuccessful for any reason, the tissue additions can simply be removed. This offers a certain amount of flexibility that isn’t available with topography-guided PRK.
CTAK Vs. Intacs
One big advantage of CTAK over Intacs is biocompatibility. A corneal tissue addition is more natural when placed in a patient’s cornea compared to synthetic intracorneal ring segments and inlays. This lessens the risk of certain complications, such as persistent corneal inflammation. Our doctors at CLEI published on the rate of Intacs removal and found that 6.1% of Intacs required removal. Specifically 2.6% had to be removed for medical complications, including sterile inflammation, a reaction to this synthetic segment.
CTAK is also much more customizable than Intacs. With CTAK, the tissue addition, as well as the channel where it is placed, is custom cut with a femtosecond laser to fit the patient’s corneal needs, which are determined by advanced corneal topography maps. Corneal mapping is used to determine where to insert Intacs as well, but the Intacs themselves are produced with fixed dimensions and cannot be custom cut like sterile donor tissue can.
CTAK Vs. Corneal Transplants
A few of CTAK’s advantages include the fact that this procedure is much less invasive and can provide significant improvements in visual acuity and corneal topography without the long recovery and potential complications associated with a transplant. In addition, CTAK tissue is gamma-irradiated. This reduces the risk of rejection compared to full corneal transplants.
Conclusion
From its inception in the research laboratory to its integration into clinical practice, corneal tissue addition keratoplasty represents a significant leap forward in the quest to improve outcomes for keratoconus patients battling this sight-threatening condition.
If you’ve been diagnosed with keratoconus, schedule an appointment with the innovators of CTAK at the CLEI Center for Keratoconus and get started on a customized, comprehensive treatment plan today.



