The corneal collagen crosslinking procedure (CXL) is designed to decrease the progression of keratoconus.
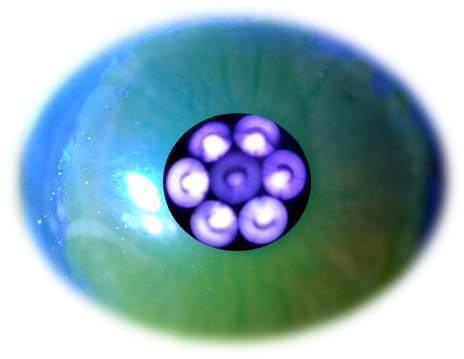
Here at CLEI Center for Keratoconus, we have been performing crosslinking for over 10 years. Crosslinking is accomplished by instilling riboflavin drops onto the cornea and then exposing the cornea to ultraviolet A (UVA – 365nm) light.
In fact, Dr. Hersh served as a medical monitor and was the lead author of the two studies leading to the U.S. FDA approvals of corneal collagen crosslinking for keratoconus and corneal ectasia.
CXL aims to halt the keratoconus disease process by strengthening the cornea. The treatment results in mechanical stiffening of the cornea, with the clinical goal being a consequent decrease in the progression of the disease process.
Laboratory studies show that immediately after CXL, strength measurements increase in human corneas by over 300%. This occurs through a relatively complex photobiologic process. When activated with UVA light in the presence of oxygen, riboflavin is converted into excited singlet and triplet states, which then undergo a series of chemical reactions resulting in the formation of reactive species that interact with corneal proteins and lead to the formation of chemical bonds.
Several different pathways lead to the formation of crosslink bonds, driven by the relative availabilities of oxygen, riboflavin, and ultraviolet light. Under aerobic conditions, singlet oxygen and hydroxyl radicals are the reactive oxygen species (ROS) produced that react with the collagen to form these bonds.
Under anaerobic conditions, radical riboflavin may also lead to the production of crosslinking molecular bonds. Balancing the competing aspects of the reaction, by controlling the rate of oxygen consumption, allows for control of the distribution of crosslinking bonds formed in the cornea.
Although these biomechanical pathways may be complicated, CXL works simply by increasing corneal strength, and in our clinical trials appears to be effective in most patients to decrease the progression of keratoconus. In addition to stabilizing the cornea, there is, on average, improvement in topographic and visual acuity outcomes.
For example, in our study of crosslinking outcomes, the topography-derived maximum keratometry (K) value flattened by 1.7 diopters (D) and patients had an improvement in corrected distance visual acuity (CDVA) from 20/45 to 20/34 and in uncorrected distanced visual acuity (UDVA) from 20/137 to 20/117.
Moreover, there was a general improvement in several corneal topography indices, corneal and total eye higher-order aberrations, and subjective patient visual symptoms. Thus, corneal collagen crosslinking offers great promise in the treatment of keratoconus of KC.
It is important to remember that crosslinking is designed to decrease disease progression, not to improve your vision. There are a number of options that can help the keratoconus patient achieve better vision. You can read about them on our other website pages.



