Corneal Transplantation Procedures
Complete Corneal Transplants (PK), Laser Assisted Transplants (Intralase Enabled Keratoplasty IEK and Femtosecond Lase Assisted Keratoplasty FLAK), Partial Thickness Lamellar Transplants (ALK, DALK)
Corneal transplantation is suggested in a number of corneal disorders including advanced keratoconus, corneal swelling, scars, and dystrophies. There are a number of different surgical options in corneal transplantation, including full thickness transplants, partial thickness transplants, and laser assisted modalities.
At the Cornea and Laser Eye Institute, we prefer the newer Intralase laser assisted procedures for many of our patients. With subspecialty fellowship training in corneal surgery and years of transplantation experience, the CLEI team works to give you the best possible option for your surgery and visual outcome.
Laser Assisted Corneal Transplant Techniques
Intralase Enabled Keratoplasty (IEK) / Femtosecond Laser Assisted Keratoplasty (FLAK)
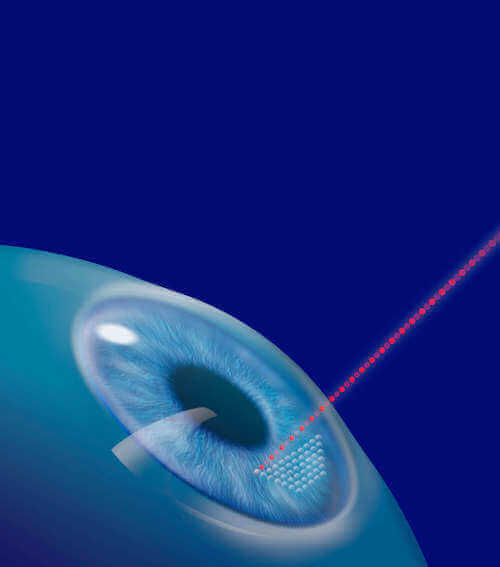
At the Cornea and Laser Eye Institute, we were amongst the first in the nation to perform laser-assisted corneal transplants. In these laser procedures, sometimes called Intralase Enabled Keratoplasty (IEK) or Femtosecond Laser-Assisted Keratoplasty (FLAK), both full-thickness (PK) and anterior lamellar transplants (ALK and DALK) can be assisted with the use of the Intralase femtosecond laser.
Rather than preparing the corneal transplant graft with a traditional trephine (a specialized circular blade) as in standard transplantation techniques, both the patient and recipient corneas are fashioned with the laser.
We find that the laser more accurately prepares the tissue, better matches the recipient to the donor tissue shape, and also can create specialized edge shapes. The result may be a faster and stronger healing of the transplant, quicker recovery of vision, and, ultimately, a better optical and visual quality of the transplanted cornea.
Laser-assisted corneal transplants are performed in two stages. In the first, the patient undergoes the IEK procedure on-site at the CLEI laser. This procedure is done under anesthetic drops and takes approximately 30 minutes.
The patient is then transported to the ambulatory surgery center, where an anesthesiologist will prepare you for the conclusion of the transplant procedure. The procedure usually takes approximately one hour and is performed with local anesthesia on an outpatient basis. After the surgery, you will go home with your eye covered by a patch and eye shield.
Full Thickness Corneal Transplantation (Penetrating Keratoplasty, PK)
In cases where the cornea has become swollen, clouded, scarred, or irregular as a result of diseases such as keratoconus, infection, or previous eye surgery, a corneal transplant is sometimes necessary to restore functional vision.
In penetrating keratoplasty (PK), the most frequently performed corneal transplantation technique, the entire cornea is removed and replaced with a donor cornea. Corneas used for transplantation have been donated to the eye bank from a deceased person.
All corneas are carefully screened and prepared by the eye bank. At CLEI, we work very closely with the Lions Eye Bank of New Jersey as well as other national eye banks.
Partial Thickness Corneal Transplant (ALK, DALK)
In anterior lamellar keratoplasty, only the front part of the cornea is replaced. This leaves the cells (called the endothelium) covering the back of the cornea intact.
By retaining the endothelial cell layer, the risk of corneal transplant rejection may be decreased, and healing may be faster. Anterior lamellar keratoplasty is suggested in conditions such as keratoconus without deep scarring or excessive thinning, and partial thickness corneal scars.
New techniques of partial thickness corneal transplantation which have been recently developed make it the preferred procedure in many cases. In particular, in Deep Anterior Lamellar Keratoplasty (DALK) technique, all levels of the cornea are replaced except for the endothelial cell layer and the membrane that holds the cells (called Descemet’s membrane).
This may improve visual quality after the transplant procedure while retaining the advantages of the partial thickness approach.
DSAEK (Descemet’s Stripping automated Endothelial Keratoplasty)
DSAEK is another type of partial-thickness corneal transplant. It is used in patients with corneal swelling caused by poor function of the interior endothelial cells of the cornea.
This swelling may be caused by problems such as Fuch’s corneal dystrophy or after other eye surgeries such as cataract surgery. In DASEK, only the back layer of the cornea is removed, consisting of the endothelial cells and the Descemet’s membrane that holds the cells.
A partial thickness of the donor cornea, containing new endothelial cells, then is implanted to replace the dysfunctional cells.
What are the chances of success?
The overall success rate of a corneal transplant is about 85%. However, there are many factors that influence the outcome. For instance, keratoconus has one of the best prognoses for good vision with a greater than 90% chance of a clear graft.
Other eye diseases such as glaucoma or retina problems may affect the visual result even if the surgery is successful. In addition, the eye must be monitored for signs of graft rejection.
In most cases, vision returns very gradually after surgery. Also, the healing process may vary greatly from one individual to the next. Some patients may enjoy improved vision within a few weeks after surgery; for others, it may take up to a year. Glasses or contact lenses are still necessary after most corneal transplants. As discussed below, a variety of vision correction procedures may also be useful.
What does surgery entail?
The procedure usually takes approximately one hour and is performed with either general or local anesthesia on an outpatient basis. After the surgery, you will go home with your eye covered by a patch and plastic shield to protect the eye.
When you see us the day after surgery, we will start your medicated eyedrops. You may use drops for a year after surgery to prevent rejection of the transplant. Stitches may remain in the cornea for several years in some cases.
Can vision be further corrected after corneal transplants?
In addition, at the Cornea and Laser Eye Institute, we have a particular interest in visual correction after transplantation. A variety of techniques may help improve vision in patients who have already had a corneal transplant. Such techniques include:
Post Transplant Contact Lenses: Specialized contact lens fitting may dramatically reduce astigmatism and improve vision after corneal transplants.
Excimer Laser PRK: In selected patients, reshaping the transplant using the photorefractive keratectomy technique can improve visual acuity without glasses or contact lenses.
LASIK: As with PRK, the LASIK technique is useful in some patients after corneal transplantation.
Conductive Keratoplasty (CK): CK uses radiofrequency energy to reshape the cornea.
Astigmatic Keratotomy: Many patients after transplantation suffer astigmatism. Revising the transplant wound, sometimes with suturing, can diminish transplant astigmatism.
All patients with corneal transplants are different. A full evaluation, therefore, is necessary to arrive at the proper plan for vision correction.



