No Flap LASEK / PRK / ASA
Laser vision correction without preparation of a LASIK flap goes by a number of names – LASEK (laser epithelial keratomileusis), surface LASIK, epithelial LASIK, epi-LASIK, or Advanced Surface Ablation, ASA).
Although LASEK and LASIK sound the same, unlike traditional LASIK, LASEK does not require the preparation of a corneal flap. This has three potential advantages:
- Risks of making the corneal flap in LASIK are avoided. This may be important in some patients in whom there is an additional risk in making the flap, such as patients with corneal scars or irregularities, patients with thin corneas, or for some job requirements. For occupational requirements, we advise you to check the requirements of the position to assure that you get the treatment that is necessary.
- Since laser treatment is done on the surface, LASEK/PRK preserves more corneal tissue. In particular, patients who have thinner corneas may be more safely treated with a no flap technique rather than LASIK
- LASEK/PRK may be an option for patients who are not good candidates for LASIK
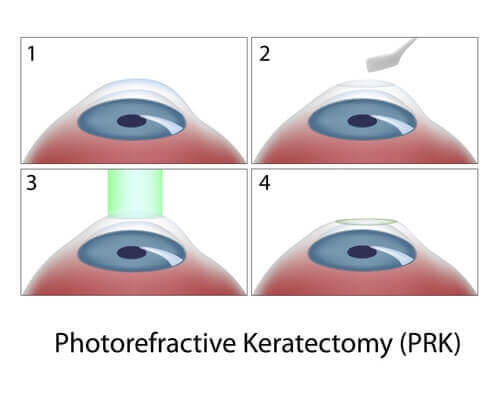
The PRK/LASEK Procedure
At the beginning of the LASEK / PRK eye surgery procedure, topical numbing drops are applied. A lid speculum holds your lids open to avoid blinking during the procedure. The surface cells of the cornea are first loosened with a solution and moved to the side.
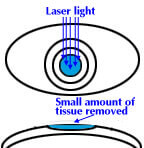
The laser treatment then is applied, taking between 20 and 60 seconds depending on the desired correction. Medications are given and, at the end of the procedure, a contact lens bandage is applied. You will use topical drops to avoid infection and control wound healing for approximately 3 weeks.
Vision after LASEK/PRK does take a little while longer to completely improve and stabilize than after LASIK. Substantial improvement usually is noticed the day after the procedure and fluctuates over the next 2 weeks.
The contact lens is removed in 5 days in most patients. Most people return to work 2-5 days after the procedure. Driving vision in the days after the procedure can be variable and take up to 2 weeks in some patients.
As with traditional LASIK, there are two basic types of possible side effects with LASEK / PRK eye surgery. Because patients may respond and heal differently, it is possible that the entire refractive error may not be corrected or that there might be some over-correction.
In this case, vision will be clearer without glasses, but less powerful glasses may still be necessary to fine-tune to your best vision. Patients who are under-corrected or over-corrected often can undergo a re-treatment procedure to further improve their vision.
In addition, like LASIK, other optical side effects include halos around lights and glare, especially at night. Other possible complications include scarring or corneal haze. We will discuss these possibilities in detail.
Frequently Asked Questions:
- Are results different from LASIK? No. Extensive clinical trials which we have published show no difference in outcomes. The only difference is the extended time for vision stabilization in surface laser procedures.
- Is the laser different from LASIK? No. The same Wavelight laser and technique are used.
- Aren’t surface procedures more uncomfortable than LASIK? Advances in surgical technique and postoperative care have made the recovery period after LASEK/PRK quite comfortable as compared with the original PRK procedure years ago.
| Item | LASEK / PRK Eye Surgery | Traditional LASIK |
| Pre-procedure examination | Similar | Similar |
| Procedural difference | Surface epithelium removed | Corneal flap prepared |
| Excimer laser procedure | Similar | Similar |
| Postoperative discomfort | Variable | Usually minimal |
| Visual recovery | Fluctuates over 1-2 weeks | Starts improving at 1 day |
| Possible side effects | Glare/halo/ghosting Corneal haze | Glare/halo/ghosting Corneal flap problems |
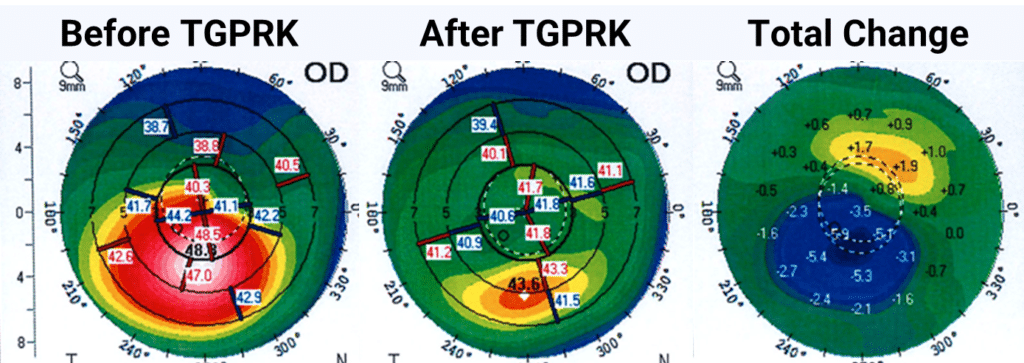
Topography-Guided PRK for Keratoconus
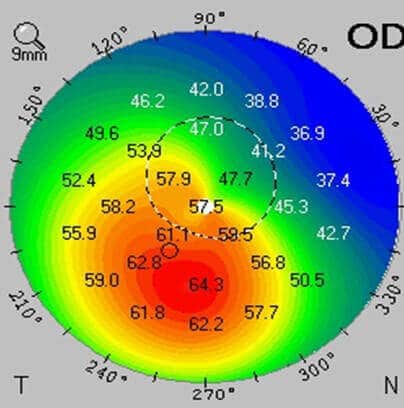
Recently, there has been much talk in the keratoconus community about combining corneal collagen crosslinking with topography-guided PRK (photorefractive keratectomy).
It is important to note, that such treatments are not FDA-approved but may be used on an “off-label” basis after consultation between the doctor and patient. Recently, we have had good success in a number of patients who were candidates for the procedure.
Usually, topography-guided PRK is used in conjunction with corneal collagen cross-linking in keratoconus, to stabilize the corneal contour over time and decrease keratoconus progression.
Topography-guided PRK uses information gained from your corneal map to program the laser to help make your cornea more optically regular. The goal of topography-guided PRK, like Intacs and CK, is to improve corneal contour in the KC patient to improve glasses corrected vision and contact lens tolerance. In general, you will still need contacts and glasses afterward.
Here at CLEI Center for Keratoconus, we have also performed adjunctive procedures on patients who have had CXL and topo-guided PRK with very encouraging results.
So, for the patient with keratoconus, it is important to know that, although KC is a chronic disease, a stepwise treatment plan can get you the best long-term vision.
Although not all procedures are for everyone, a tailored approach over time may combine a variety of procedures to optimize your corneal shape and visual outcome.
Other in-depth articles and studies related to LASEK/PRK:
Introduction to the Excimer Laser
Results of Phase III Excimer Laser Photorefractive Keratectomy for Myopia
Characteristics Influencing Outcomes of Excimer Laser Photorefractive Keratectomy
In the News:
At Issue: preferred regimen for curing haze after PRK – June 15, 2000
From Dr. Hersh’s book:
Ophthalmic Surgical Procedures
Chapter 23. Photorefractive Keratectomy (PRK)/Laser Epithelial Keratomileusis (LASEK)
Indications
- Surgical correction of natural myopia, hyperopia, and astigmatism.
- Selected cases of postsurgical myopia, hyperopia, and astigmatism.
- Selected cases of presbyopia management with a monovision outcome.
- Selected cases of thinner corneas in which LASIK contraindicated.
- Selected cases of epithelial basement membrane dystrophy.
- Vocational needs (occupations in which LASIK flap not allowed).
Contraindications
- Keratoconus and forme fruste keratoconus.
- Collagen vascular diseases and inflammatory ocular diseases.
- Herpes keratitis.
- Pregnancy.
Preoperative Procedure
- Discontinue soft contact lens wear at least 1 week and rigid contact lens wears 2 weeks preoperatively. Confirm the stability and regularity of corneal topography.
- Do not wear eye makeup days of the procedure.
- Treat pre-existing dry eye and blepharitis. Consider nonpreserved lubricants, lid hygiene, punctual plugs, topical cyclosporine, and oral doxycycline for blepharitis.
- Optional: Administer oral corticosteroid day of procedure and taper thereafter to decrease postoperative discomfort.
- Assure appropriate corneal thickness with ultrasonic pachymeter (Note: Corneal thickness-ablation depth should leave >350 microns to minimize the risk of corneal ectasia. This number is a suggestion and has not been validated)
Instrumentation
Lid speculum
Cellulose sponges
Epithelial removal instrumentation:
- Spatula
- Amoils epithelial brush
- 20% EtOH with 8-9 mm optical zone marker “bath”
- Epithelial microkeratome
Mitomycin C 0.02% (optional)
Therapeutic soft contact lens
Procedure
- For lasers requiring pupil dilation, administer tropicamide 1% +/- phenylephrine 2.5%.
- Prep and drape operative eye.
- Place lid speculum.
- Remove corneal epithelium over an 8-9 mm area using one of the following techniques:
- Mechanically scrape with a spatula.
- Mechanically remove with Amoils epithelial brush.
- Place 20% EtOH for approximately 20 seconds in an 8-9mm optical zone marker bath (Fig. 23–1).
- Irrigate residual EtOH with a chilled balanced salt solution.
- Loosen epithelium with a cellulose sponge.
- Remove epithelial sheet with cellulose sponge or spatula (Fig. 23–2)
- Elevate epithelial flap with an epithelial microkeratome. For techniques (c) and (d), above, the flap may be discarded or repositioned after the laser ablation.
- Gently wipe bed with cellulose sponge or spatula to remove residual fluids.
- Engage laser eye tracker and align laser as necessary
- Alignment technique varies with the laser platform
- Center over pupil
- Encourage patients to maintain gaze at a fixation target.
- Perform laser ablation (Fig. 23–3).
- Irrigate surface with chilled balanced salt solution or lactated Ringer’s solution (chilled solution aids in minimizing discomfort postoperatively).
- Reposition epithelial flap if desired.
- Apply a therapeutic contact lens.
- Administer corticosteroid and antibiotic drops.
- Remove lid speculum.
Postoperative Procedure
- Corticosteroid drops four times per day for one week and taper to two times daily for one week and one time daily for one week
- Topical antibiotic four times per day for one week.
- Nonpreserved lubricants as needed.
- Taper oral corticosteroid if used.
- Topical and oral nonsteroidal anti-inflammatory agent for pain control as needed.
- Oral narcotics for pain as needed.
- Optional: Vitamin C 1000 mg daily (may aid in corneal haze prevention).
- Explain postoperative management to patients.
Follow-Up Schedule
- Postoperative day 1.
- Postoperative day 3-5 (general examination with attention to epithelial healing and contact lens removal).
- Month 1.
- Month 3 (full exam to assess the status and consider retreatment if necessary).
- Months 6, 12 as necessary.
Complications
Early Postoperative Complications
Poor epithelialization.
Intermediate-Term Complications
- Epitheliopathy.
- Corneal haze.
Late-Term Complications
- Over and under corrections.
- Induced astigmatism.
- Induced topography irregularities.
- Corneal haze.



