The CLEI Center for Keratoconus is world-renowned for innovating and improving upon corneal surgical techniques. One such technique is corneal tissue addition keratoplasty (CTAK). Unlike treatments that simply focus on addressing refractive errors, CTAK was envisioned as a procedure that could address the underlying structural irregularities associated with keratoconus. In 2016, clinical trials for this groundbreaking technique began, with some outstanding results. How does it work? We’ll break down the science behind this innovative technique that was developed right here at CLEI. We’ll also answer a few commonly asked questions about the procedure.
What is CTAK?
CTAK is a form of lamellar keratoplasty invented with keratoconus patients in mind. Keratoconus causes the cornea to thin and bulge, developing a steep cone shape over time that can severely impact a person’s vision and quality of life. Unlike a full corneal transplant, or penetrating keratoplasty, CTAK involves adding a custom-shaped, irradiated corneal tissue inlay to the patient’s own cornea through a channel created by a femtosecond laser. CTAK results in the reshaping of the patient’s cornea for improved vision.
Corneal Tissue Addition Keratoplasty Explained
In preparation for CTAK, we use multiple devices to map your cornea. This tells us the exact curvature and elevation of the cornea. We input this information into specialized software, designed right here at CLEI, to create a personalized surgical plan for optimal tissue placement. We then use a femtosecond laser to cut the tissue inlay to the proper width, diameter, length, and angle, to meet your specific needs. This customization allows CTAK inlays to be used in mild, moderate, and even severe cases of keratoconus with excellent results.
Once the inlay is prepared, you can come in for the surgery. Before we begin, numbing drops are applied to your eye so you will remain comfortable and pain-free during the procedure. Next, we use the femtosecond laser to create a channel in a precise location in your cornea. The channel is just the right size to fit the tissue inlay. Using surgical tools, we insert the corneal tissue inlay into the channel to add thickness to the cornea and decrease the irregular cone shape. This entire procedure takes less than 30 minutes.
After the procedure, you’ll be given a corticosteroid drop to prevent inflammation and antibiotics to prevent infection. Within a week of the procedure, most patients see improvement in their vision. You’ll need to attend follow up appointments to make sure your eye is healing well and adapting to the tissue inlay.
While CTAK does improve uncorrected vision, it’s worth noting that in most cases it is used to correct vision in glasses and contact lenses. About one month after the surgery, your CLEI eye care specialist will check your glasses or lens prescription and update it as needed.
Frequently Asked Questions About Corneal Tissue Addition Keratoplasty
Who is CTAK for?
CTAK was developed for keratoconus patients. While it is not a cure for keratoconus, for many patients, it plays a vital part in their overall keratoconus treatment plan by improving the keratoconus topography.
What if my doctor said my only option is a corneal transplant?
We would encourage you to come in for an evaluation at CLEI. Our experienced eye surgeons are the pioneers of and the innovators behind the CTAK procedure. For many patients, CTAK, which is much less invasive than a full corneal transplant, may be a viable alternative to a full corneal transplant.
Where does the tissue come from?
The tissue used in CTAK is harvested from a donor after meeting all criteria of the Eye Bank Association of America (CorneaGen, USA). It is frozen to inactivate the cells, then sterilized with gamma irradiation. This process eliminates the donor cells leaving only the collagen lamellae of the cornea for implantation. Over time, the patient’s cornea cells have been shown to repopulate this tissue. This means rejection of these inlays is very unlikely.
What are the potential risks of CTAK?
All surgical procedures carry some potential risks like infection, inflammation, or scarring. We minimize these risks with antibiotics and a postoperative corticosteroid drop. One other potential, albeit rare, risk is the potential for unexpected or worsened corneal shape. This can be addressed by removing the corneal tissue addition, reshaping it, and performing CTAK a second time.
Is CTAK reversible?
Yes. One big benefit of this procedure is the fact that it is completely reversible. Should an issue arise, we can simply remove the corneal tissue addition.
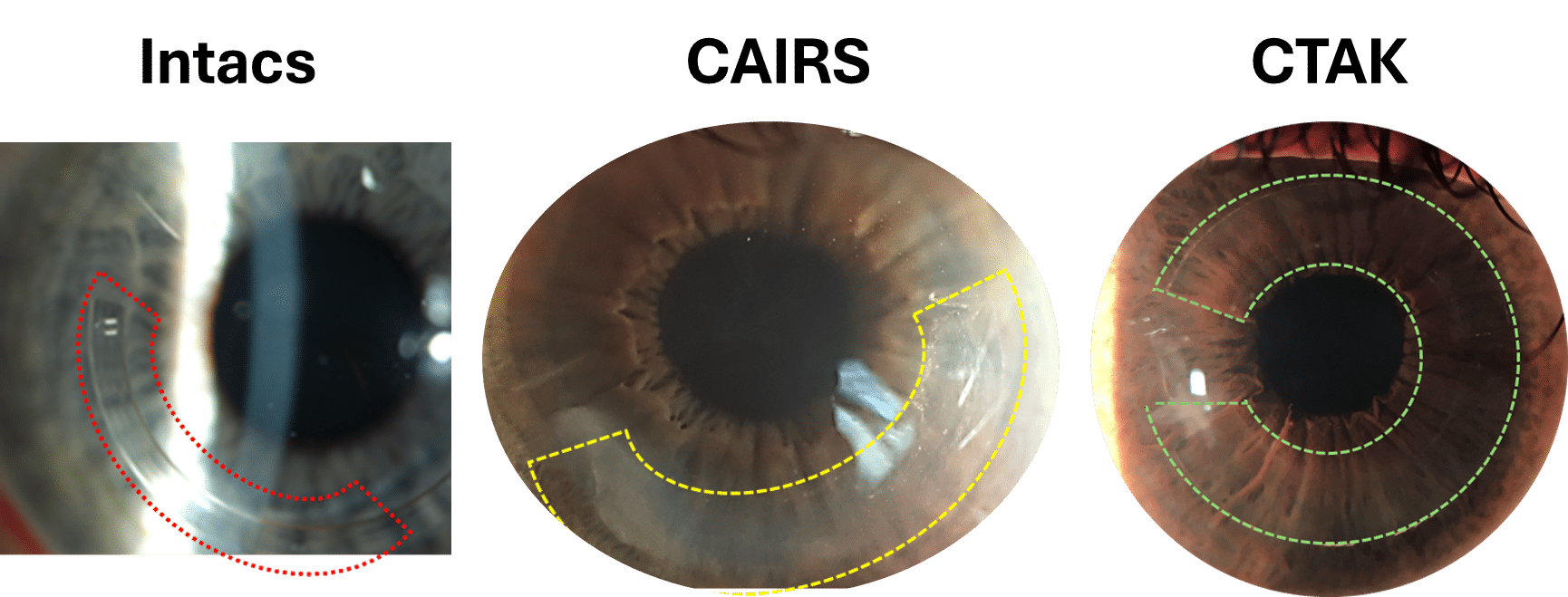
How is CTAK different from Intacs?
Intacs are synthetic intracorneal ring segments and inlays designed to improve the corneal shape. Because they are synthetic, they are less biocompatible than a CTAK inlay. Like the CTAK process, corneal mapping is used to determine where to insert Intacs, however, the Intacs themselves are pre-produced with fixed dimensions. They cannot be custom cut like sterile donor tissue can. In fact, for patients in whom Intacs did not achieve a satisfactory result, here at the CLEI center for keratoconus, we have been able to replace these Intacs segments with CTAK inlays with improved visual acuity results.
Is CTAK the same as CAIRS?
No. While there are similarities between the CAIRS (Corneal Allogeneic Intrastromal Ring Segments) and CTAK procedures; for example both use corneal tissue to create the inlay, the development of CTAK and CAIRS were fundamentally different. CAIRS was developed to imitate synthetic intrastromal corneal ring segments such as Intacs and were made out of corneal tissue for improved biocompatibility. CTAK on the other hand was designed as a visual axis sparing lenticule which is custom shaped by a femtosecond laser and positioned to ameliorate a patient’s individual corneal shape.
Conclusion
If you’ve been struggling with keratoconus, or if you’ve been told a corneal transplant is your only treatment option, we invite you to schedule an appointment at the CLEI Center for Keratoconus today. We are dedicated specialists who can help you explore the latest technology and treatment options available for keratoconus patients. We understand that your vision is inextricably linked to your quality of life, and we aim to help you attain and enjoy the best vision possible.